Abstract
Increasing evidence shows that nutrition plays a role in the pathogenesis and progression of many diseases. Certain diets are shown to play a role in driving systemic inflammation and consequently contribute to exacerbation of disease processes. Systematic nutrition assessment in individuals with sickle cell disease (SCD) is largely unexplored and thus it is not well understood how diet impacts SCD complications and health outcomes. Therefore, the objective of this study was to assess both the inflammatory nature and quality of diet in adults with SCD.
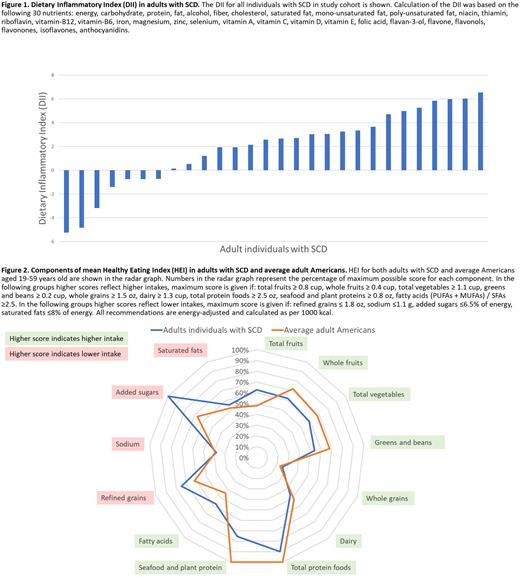
Individuals with SCD age ≥18 years were eligible for enrollment. Consented participants completed the validated diet assessment, the Block 2014 Food Frequency Questionnaire. This questionnaire has a recall period of one year and includes questions on the intake of 127 food and beverage items. Data collected from this questionnaire are sent to the developer for secondary and tertiary analyses for quantification of nutrients and food groups and the returned quantifications were used to calculate the Dietary Inflammatory Index (DII) and the Healthy Eating Index (HEI). The DII is a validated measure that quantifies the inflammatory nature of individuals' diet based on the potential of nutrients to trigger inflammation, whereas the HEI is a metric that assesses overall diet quality and several individual dietary components. DII is calculated based on the global mean intake and standard deviation (SD), and overall inflammatory effect score for specific food parameters. A total of 30 food parameters (Figure 1) were used for DII calculation in this study. Global mean intake and SD are used to calculate a Z-score for each nutrient which is then converted to the centered percentile. It is then multiplied with the overall food parameter-specific inflammatory effect score from the DII database to get a DII for each nutrient. These individual nutrient scores are summed to create the 'overall DII score' for an individual. Possible overall DII scores range from -8.87 to +7.98, with negative scores indicating an anti-inflammatory diet and positive scores indicating a pro-inflammatory diet. The HEI reflects adherence to Dietary Guidelines for Americans (DGA) and considers density-based (amounts per 1,000 kcal) intake of the following 13 components: total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars, saturated fats. Fruits, vegetables, and proteins are assigned a maximum of 5 points each because they are represented by two components (i.e., total fruits and whole fruits) while other food groups receive a maximum of 10 points because they are represented by one component. Maximum points are assigned if the a priori set thresholds for the specific components are met (detailed in Figure 2 legend). Final HEI is a sum of scores for each component. The HEI has a range of 0 (reflecting no adherence to DGA) to 100 (reflecting complete adherence to DGA). The mean HEI for Americans aged 19-59 years old is 57. We report the range and mean for both the DII and HEI indices.
A total of 28 adults with SCD completed the Block Food Frequency questionnaire. Mean age of participants was 33.7 (SD 10.5) years with range of 19-58 years and 46.4% (n=13) were female. Figure 1 represents the DII scores for our study cohort. We found 25% (n=7) of individuals had a negative DII indicating consumption of an anti-inflammatory diet, and 75% (n=21) of individuals had a positive DII indicating consumption of a pro-inflammatory diet. The DII ranged from -5.25 to 6.55, with a median DII of 2.62 (IQR -0.49, 4.45). The mean HEI score for the study cohort was 60. Individual components of the mean HEI for SCD individuals and for average adult Americans are shown in Figure 2. Numbers in the radar graph represent the percentage of maximum possible score for each component.
The majority of adults with SCD in our cohort have evidence of a pro-inflammatory diet. Our cohort had a similar HEI to average Americans, but its components vary between the food groups and require further assessment. These data are the first step to systematically assessing nutrition in individuals with SCD. Further research is necessary to investigate if nutrition impacts disease expression and health outcomes in SCD and determine whether diet is a modifiable target for interventions.
Disclosures
Hankins:GBT: Consultancy; Forma Therapeutics: Consultancy; CVS Health: Consultancy; NHLBI: Membership on an entity's Board of Directors or advisory committees, Research Funding; CDC: Research Funding; HRSA: Research Funding; ASH: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal